Object: Chimeric Antigen Receptor T-Cell (CAR-T) therapy has been developed to be the most effective treatment for relapse and refractory(R/R) B-cell acute lymphoblastic leukemia(B-ALL). However, in some patients prolonged chemotherapy and previous autologous-CAR-T(auto-CAR-T) therapy severely impaired lymphocyte function leading to inability in vitro expansion for effective CAR-T therapy. To address this challenge, we designed this clinical trail to use one-stop no-edited allogenic CAR-T(allo-CART)bridging to same donor conditioning free HSCT to treat children with R/R B-ALL.
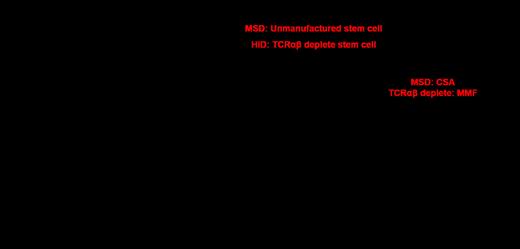
Methods: Myeloablative conditioning was given to reducing the leukemia burden and clearing lymphatic function for these active ALL. After that allo-CART was used to regain the immune killing effect and clear leukemia cells. Same donor seamless conditioning free HSCT were performed to rapid reconstruction of hematopoietic cells to overcome Immune effector cell associated hematologic toxicity post CAR-T therapy. Ex vivo TCRαβ+ T-cell depleted hematopoietic stem cell were transplanted for haplo-identical donor (HID) to minimize allogeneic reactivation and only macophenolate mofetil (MMF) were given for GHVD prophylaxis and to avoid more immunosuppressive to injury CART effect.
Results: From October 2020 to April 2023, 16 extremely R/R B-ALL children with the median age of 10y (1.5-17) were recruited in this study, all patients relapsed 2-5 times and failure of 1-3 times auto-CART therapy with mean blast 70.6%±28.8%. Myeloablative conditioning with total body irradiation (12GY,-7d to -5d),Flu (160mg/m2, -5 to -2d) and CTX (120mg/kg,-4d to -3d) were given. After conditioning all patients received no-edited family donor allo-CAR-T therapy with the average cart (5.29±2.92)×10 6/kg, 3 from matched sibling donor (MSD) and 13 from haplo identical donor(HID). 6 patients received CD22-targeted CAR-T therapy due to loss of CD19 after previous auto-CART and another 10 received bispecific CD19/CD22-targeted CAR-T therapy. Immediately after the peak of cytokine release syndrome (CRS), median 11 days (range: 8-34 days), same allo-CART donor hematopoietic stem cell were transplanted with the median CD34+cells(6.88±2.77)×10 6 /kg and TCRαβ+T cells(18.65±16.10)×10 4 /kg for TCRαβ+depleted HSCT. After median follow-up of 8 (range 3 to 34) months for the surviving patients. Out of the 16 patients, 6 (37.5%) achieved CR after conditioning, 13 (81.3%) achieved CR after CAR-T therapy and 15 (93.8%) got CR at one month post HSCT. Among the 16 patients, 15 experienced CRS (above grade 1) and one accompanied by immune effector cell-associated neurotoxicity syndrome (ICANS), but no one died of CRS. 13(81.2%) patients developed acute graft-versus-host disease (aGvHD) before transplant mainly presented with skin GVHD except 3(18.9%) had a grade III GVHD which easily be resolved. Before HSCT, all patients achieved complete chimerism with donor T-cells. Almost every one experienced several episode infection during these therapy. Until the last follow-up, 2 cases relapsed and 5 died (2 died of infections, 1 died of relapse and 2 died of GvHD combined thrombotic microangiopathy and infection). Despite being a cohort of R/R patients with non-CR, the estimated overall survival (OS) at 1 year was 58.7%±16.0%, event-free survival (EFS) was 44.4%±14.2%.
Conclusion: For children with repeated relapsed B-ALL failure of previous auto-CART, Allo-CART treat can be considered as long as CART targets still presented. One-stop no-edited same donor allo-CART bridging to conditioning free HSCT provides a chance of survival for these extremely refractory/relapsed B-ALL with manageable CRS and GVHD, but more serious infection.
Disclosures
No relevant conflicts of interest to declare.